Apostolos Bozis discusses a recently referred endodontic case.
This 14-year-old female patient had presented to her regular dentist with pain, following the development of an abscess on her upper right lateral incisor. The tooth was diagnosed with apical periodontitis and endodontic therapy was performed at this time. However, the tooth failed to settle down completely and remained intermittently symptomatic.
Five years later, the patient experienced severe pain and swelling around the tooth, prompting a return to her dentist. Clinical examination and a LCPA radiograph confirmed that the previous endodontic treatment had failed and the patient was subsequently referred to me at Ten Dental+Facial.
A full clinical assessment was conducted during the initial consultation, which found the patient to have very good general oral health, with no previous restorations or other concerns. The shape of the clinical crown of the tooth was rather uncommon with a deep invagination and the relevant periapical radiograph, in combination with the CBCT scan, revealed quite irregular root canal anatomy of the tooth in question. The final diagnosis was apical periodontitis of upper right lateral incisor with ‘dens invaginatus’.
Dens invaginatus
This is a developmental malformation of teeth in which there is an infolding of the dental papilla during tooth development, or invagination of all layers of the enamel organ into the dental papilla before calcification is complete. For teeth that are affected, this can cause severe infolding of enamel and dentine, starting from the tip of the cusps and extending deep into the root resulting in a second opening at, or near, the root apex. This malformation was first described by a dentist called Socrates back in 1856, but Hallet is credited with
introducing the term ‘dens invaginatus’ in 1953. Other terms that were used to describe this malformation include
dens in dente, invaginated odontoma, dentoid in dente and tooth inclusion.
Prevalence of dens invaginatus has been reported to range between 0.04-10 per cent of the global population. Most commonly affected are the lateral incisors, accounting for 42 per cent of all cases. In 43 per cent of cases, dens invaginatus can be bilateral, hence clinicians should always check the contralateral tooth.
The causes of the condition are unclear, but several theories have been suggested such as infection; trauma; growth pressure of the dental arches during odontogenesis causing infolding of the enamel; and rapid proliferation of the internal enamel epithelium that invades the underlying papilla. Genetic factors could also be responsible. During tooth development, growth molecules have been shown to regulate the folding and development of the enamel organ. If those factors are absent or altered, then the morphology of developing teeth could be disturbed. This theory is supported by the fact that dens invaginatus can have a familiar tendency among parents and siblings and the lesions are also associated with other genetically determined anomalies.
Many attempts have been made to classify dens invaginatus but the most widely used system is that produced by Oehler (1957). This system separates the lesions into three simple categories:
Type I: An enamel-lined minor channel, which is formed within the crown but not beyond the amelo-cemental junction, and it doesn’t involve the pulp.
Type II: An enamel formed channel, which invades the root, but remains in a blind sack with no communication with the periodontal ligament. It may communicate with the pulp.
Type III: A form that penetrates through the root, perforating at the apical area showing a ‘second foramen’ in the apical or periodontal area. There is no immediate communication with the pulp. The invagination may be completely lined by enamel or, more commonly, by cementum.
Diagnosis of the condition requires a thorough clinical and radiographic examination for identification of:
- An abnormal shape to the crown of the tooth
- A conical-shaped tooth
- An exaggerated talon cusp
- A deep pit on the lingual side of the tooth
On the periapical radiograph, the invaginatus tissue could appear as a translucent pocket, larger lesions can appear as fissures, the pulp can be involved and the root canal will feature complex anatomy. In addition, where bilateral incidences are detected in one tooth, the contralateral tooth should be investigated.
In modern dentistry, a CBCT scan is a very important tool in diagnosing dens invaginatus, as it provides the clinician with a highly detailed 3D image that aids the treatment planning procedure.
The best treatment option is prevention. Therefore, if this malformation is detected and the tooth is asymptomatic, clinically and
radiographically vital, with no evidence of pathology, a preventive approach should be taken. This involves the seal of the invaginated pit with resin composite or fissure sealant, followed by regular reviews.
If the tooth becomes infected then further intervention would be required. The options could include conventional endodontic therapy, surgical endodontics or even extraction if a predictable treatment result with a good long-term outcome cannot be achieved.
The final decision is taken after considering the following factors:
- The stage of the root development
- Configuration of the root canal system
- Aesthetics and function
- Patient choice and co-operation
This case
In this case, the previous endodontic therapy had failed as the complicated root canal network was not addressed effectively. After clinical and radiographic examination, diagnosis of apical periodontitis was reached. There was a deep invagination that communicated with the main canal, hence it was a type II dens invaginatus. However, the careful inspection of the CBCT scan provided further valuable information regarding the complex root anatomy. Two additional canals and their exact position were detected, a fact that could dictate the treatment approach.
Treatment options discussed were:
- Revision of the failed root canal treatment, under an operative microscope, during which the complex root canal anatomy would be explored and treated
- Periapical surgery
- Extraction and replacement of the tooth
- Do nothing and monitor
After a lengthy conversation with the patient where all possibilities were evaluated and advantages and disadvantages were explored, it was decided to approach the problem in the most conservative way – hence, option one was selected.
The endodontic therapy was carried out in two sessions with local anaesthetic, under rubber dam isolation and using the operative microscope. In session one, access was gained into the root canal network and the old root filling material was dismantled using K-files and the appropriate GP solvent (Eucalyptus oil). As already suspected after having seen the CBCT sections, two additional canals were located in a more palatal position compared to the main canal. No vital pulp tissue was seen and all three canals were chemo-mechanically prepared following the standard protocol with sodium hydrochloride (which was ultrasonically activated) and EDTA 17 per cent, before being dressed with calcium hydroxide. The access cavity was temporised with IRM.
During the second session, the patient was symptom-free. The root canal network was re-accessed and further irrigated before being obturated with the continuous wave of condensation technique, together with GP and AH plus sealer (Dentsply). A layer of IRM was placed over the GP and the access cavity was sealed with glass ionomer.
The patient was completely asymptomatic from the second appointment onwards, ensuring her satisfaction with the treatment provided. CBCT and post-operative radiographs were taken, and the patient was scheduled to be reviewed in due course.
For cases like this, the use of an operating microscope is imperative and the relevant imaging technology (radiographs and CBCT) can provide all the needed pre-operative information. Cases like these can be addressed in a more predictable way for increased satisfaction of the patient and the practitioner.

Fig 1. Pre-operative radiograph. The off-centred position of the current root filling is a strong indication of missed canal(s).

Fig 2. Buccal aspect of the lateral incisor. The unusual anatomy of the clinical crown is evident.

Fig 3. Occlusal aspect of the lateral incisor. Another view of the unusual morphology of the clinical crown.
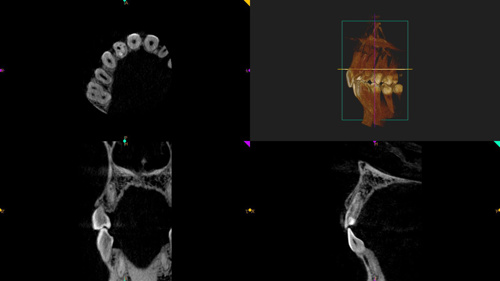
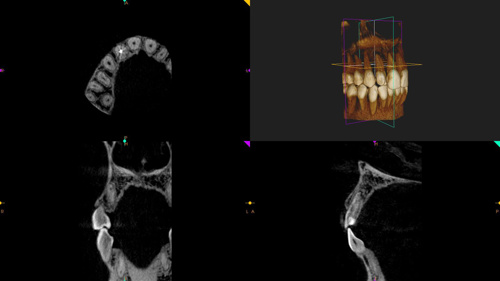
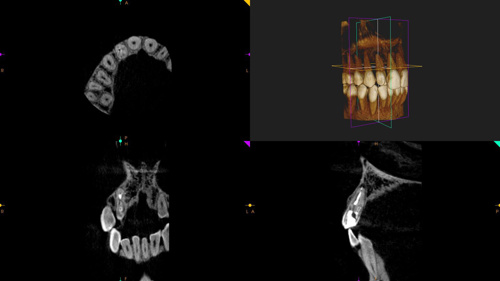
Figs 4a-c. Snapshots of the CBCT scan. The complicated root canal anatomy is visible with two smaller additional canals towards the palatal aspect and the already filled canal, which is positioned more buccally.

Fig 5. View of the access cavity after the removal of the previous root filling material and chemo-mechanical preparation. The three canal orifices are apparent.

Fig 6. Cone fit radiograph. The main wide canal and the two additional ones can be seen.

Fig 7. View through the access cavity after the obturation.

Fig 8. Post-operative radiograph. The three canals are obturated down to their apices.

