Immediate implants have been shown to deliver highly positive outcomes in a broad range of situations. No significant differences in survival rates have been identified between implants placed using delayed and immediate protocols. The literature also supports immediate loading, with research demonstrating high survival rates once again.
Further advantages can be experienced when a digital workflow is implemented, as the approach has been proven to afford several benefi ts impacting both the clinician and patient. These include shorter treatment times, a simpler professional workflow, more efficient lab work and reduced operating costs.
The following case report shows the successful outcomes that can be achieved with a combination of immediate protocols and a digital approach.
Case presentation
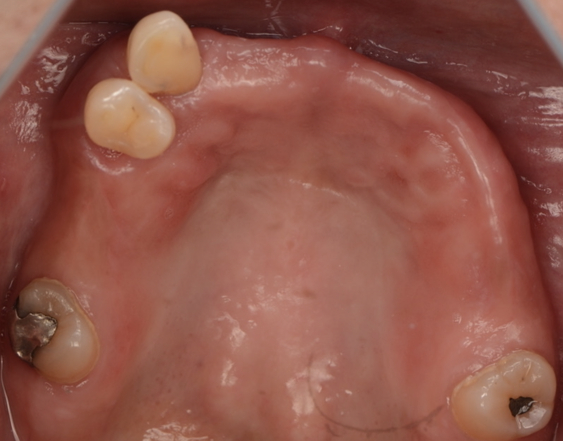
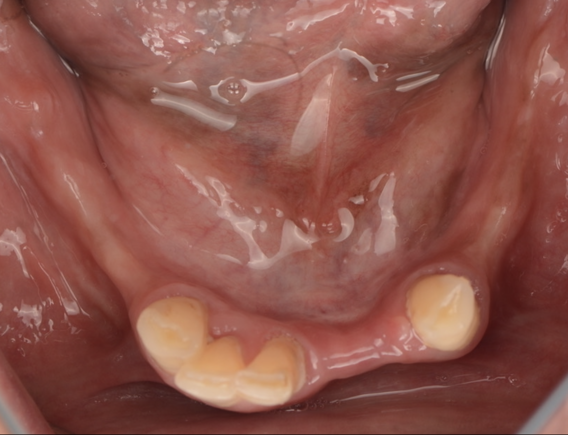
A 61-year-old female presented with a long history of wearing removable partial dentures in both the maxilla and mandible. The mandibular partial denture was particularly ill-fitting, making it difficult for her to eat comfortably.


Treatment plan
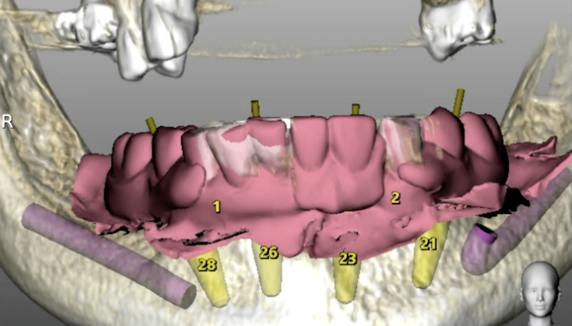
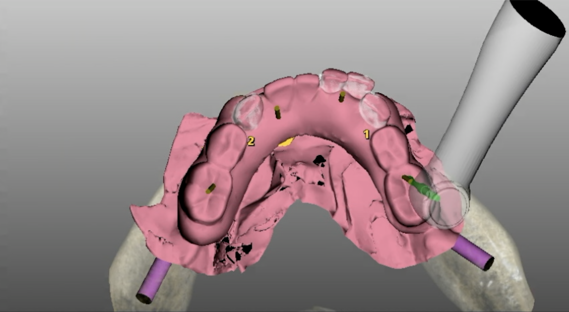
A collaborative treatment plan was developed by a multidisciplinary team which consisted of two prosthodontists (Fernando Rojas Vizcaya and Kia Karimi) and myself, a periodontist. The plan involved extracting the remaining mandibular teeth and immediately placing and loading implants. Concurrently, a digital workflow was implemented to design both the provisional mandibular prosthesis and an improved maxillary prosthesis.
To facilitate accurate implant placement and prosthesis delivery, a duplicate of the mandibular prosthesis was 3D printed with an open occlusal design, ensuring correct orientation of the multi-unit abutments. Additionally, a prosthesis positioning guide was fabricated to aid in proper seating of the mandibular prosthesis, compensating for the loss of anatomic landmarks following flap elevation and bone reduction.
Surgical procedure
The implant surgery and immediate loading was conducted during a live surgery demonstration at the Vista Institute for Therapeutic Innovations.
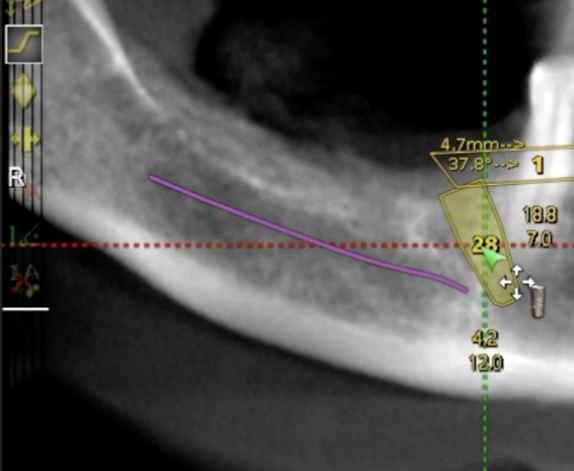
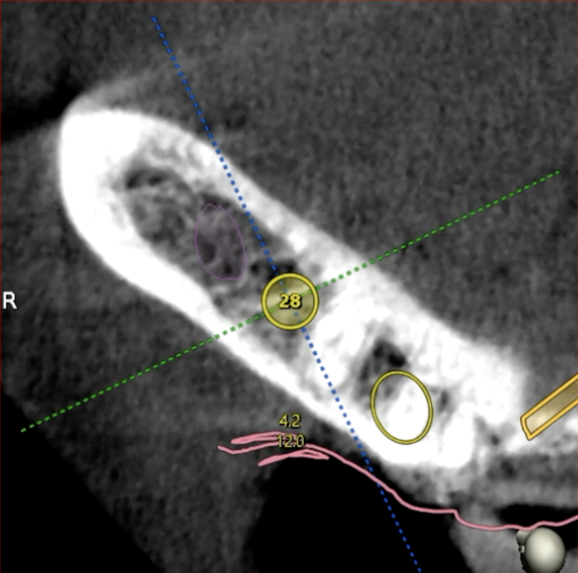
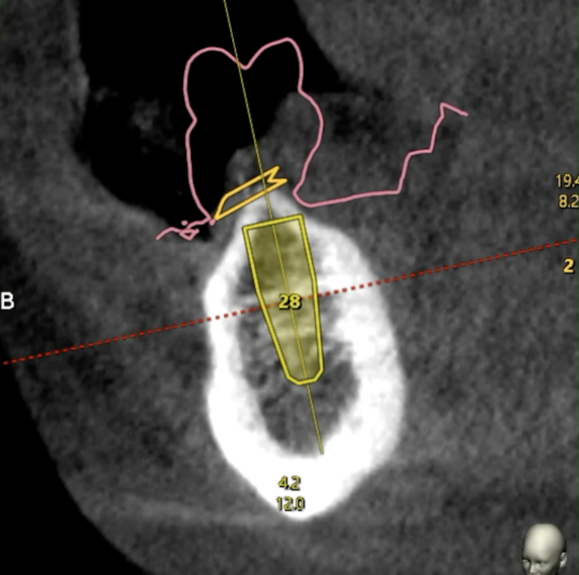
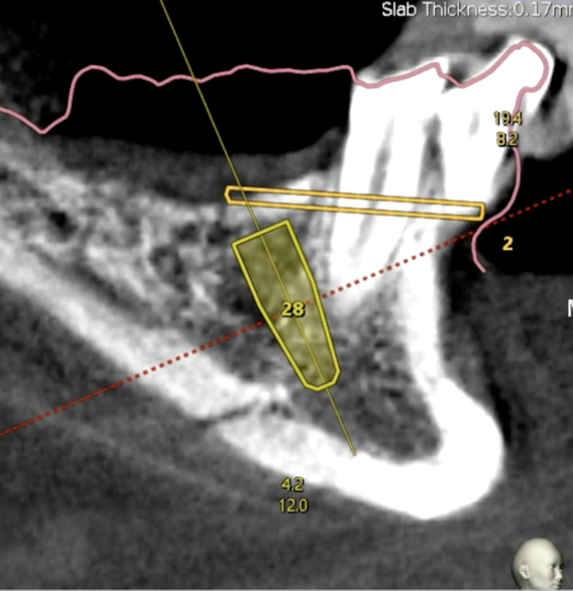
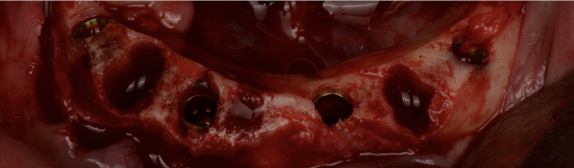
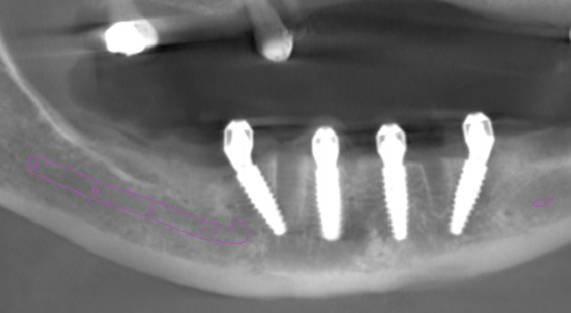
Osteotomies were performed using dynamic navigation, which provided precise control over implant positioning in accordance with the preoperative plan. The navigation system tracked jaw position using a navigation tracker placed on the remaining anterior teeth, allowing accurate placement of the posterior implants which were not covered by the tracker. Subsequently, a second tracker was fixated to the mandibular symphysis to transfer the registration data to a bone-fixated tracker after the extractions.
The implants used were BioHorizons Camlog Tapered Pro Conical, chosen for their deep conical connection, which promotes a secure implantabutment seal. This allowed for placement 1-2mm subcrestally to optimise stability.
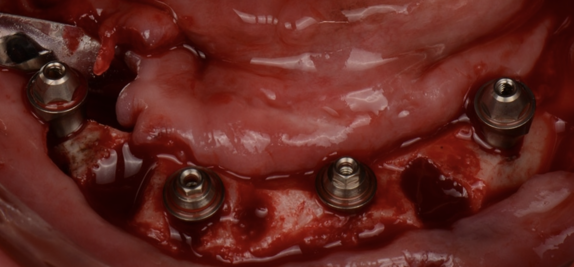
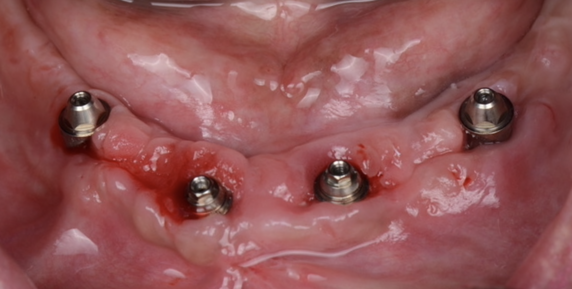
Straight multi-unit abutments (MUAs) were placed on the anterior implants, while 17-degree angled MUAs were used for the posterior implants. All abutments were torqued to 20Ncm. Implant positions were then recorded using photogrammetry to ensure precise prosthetic fabrication.
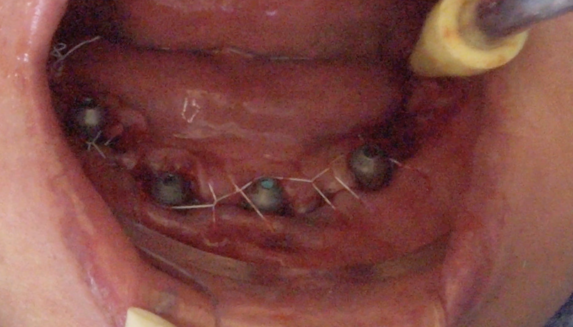
Following implant placement, BioHorizons MUA healing caps were secured, and the surgical site was closed with continuous interlocking PTFE sutures. An intraoral scan was performed to capture the peri-implant soft tissues.

Prosthetic workflow
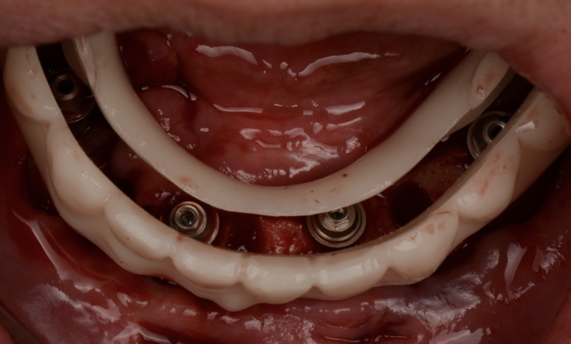
To register the occlusion and vertical dimension, the MUA guide was filled with polyvinyl siloxane bite registration material and seated using the prosthesis positioning guide. Once the material had set, an intraoral scan was taken to capture the bite and vertical dimension.
The patient was given a short break while the dental technician designed the provisional prosthesis. The design was reviewed by the periodontist and prosthodontists, who provided feedback before approving the final STL file. The provisional prosthesis was then 3D printed in OnX Tough 2, a resin reinforced with ceramic for added strength.
The provisional prosthesis was delivered with minimal adjustments, ensuring a comfortable and functional immediate restoration.


Postoperative phase and definitive prosthesis
The patient was closely monitored throughout the healing period, which proceeded uneventfully. Once osseointegration was confirmed, another intraoral scan was performed to capture the healed peri-implant tissues and to refine the prosthetic design.
A monolithic zirconia prosthesis was then milled and delivered, providing a durable and aesthetic final restoration.
This case highlights the advantages of a fully digital workflow, combining dynamic navigation, photogrammetry, intraoral scanning, 3D printing and an implant with deep conical connection to achieve a predictable and efficient outcome in immediate implant rehabilitation.



References available on request.
For more information visit https://theimplanthub.com


